The Promise of TMS, A New Path for Mental Health Recovery


What happens when conventional mental health treatments don’t work? For Tag Frothingham, the answer came in the form of transcranial magnetic stimulation (TMS)—a groundbreaking, non-invasive therapy that uses magnetic fields to stimulate nerve cells in the brain, offering new hope for those battling depression and other mental health challenges.
In this episode of This Way Up, Tag shares his extraordinary journey of overcoming severe depression, surviving cancer twice, and navigating a lifelong battle with mental health. He opens up about the frustrations of traditional treatments, the life-changing impact of TMS, and how this therapy has also supported his children’s mental health.
This inspiring conversation highlights the transformative potential of TMS, the importance of advocating for innovative care, and the role of resilience in navigating life’s toughest moments.
Don’t miss this compelling story of courage, hope, and the future of mental health care.
BIO:
Tag Frothingham is a husband and a dad of two teenagers who lives in Harvard, Massachusetts. He lives with depression and also provides support for family members with depression and anxiety. Tag is also a cancer survivor. Although he has worked in software engineering and quality assurance roles for technology companies for most of his career, he worked as a residential counselor while attending Wheaton College and for a few years after. Mental health has remained an important cause for him. In his spare time, you’ll find Tag reading, cooking, riding his bike, or playing with the family dog.
RESOURCES/ REFERENCES:
Families for Depression Awareness: https://www.familyaware.org/
Facebook and Instagram: @familyaware
Transcranial Magnetic Stimulation: TMS
Disclaimer: The information provided in this podcast is for educational and informational purposes only and should not be considered as professional advice. Listeners are encouraged to seek guidance from qualified professionals for their specific situations.
The odds of it working are decent. I mean, they're not great, great. It's worth the shot. It's worth a shot. I agree. It is super low effort. I mean, you, you spend more time in the car quite often than you do at the appointment. That was true with us. Yes.
Welcome to This Way Up, the podcast dedicated to supporting parents and caregivers navigating the complex world of mental health. I'm Andrea, and each episode, we dive deep into the conversations that matter, exploring the challenges, triumphs, and transformative journeys of those facing mental health struggles within their families.
Whether you're here for expert advice, inspiring stories, or just a little boost to get you through the day, we've got you covered. So grab a cup of coffee, kick back, and join us as we find the bright spots in the mental health journey, because we're all climbing our way up together.
Welcome back. It's Andrea, and thank you so much for joining us today. Today, we are joined with Tag Frothingham, who shares an incredible story of resilience and hope. Tag, as a young child, was diagnosed with severe depression and lived with it the majority of his life until he got cancer twice and was recommended a new treatment.
called transcranial magnetic stimulation, or TMS. Tagg shares with us very openly what it's like to live with severe depression, how it affects his daily life, how it affects his social life. And then he also shares with us how TMS changed his life for the better and really gave him joy and purpose for the future.
I hope you enjoyed this episode as much as I enjoyed speaking with Tag. If you did, please subscribe and share this with anyone that you think this might help. Thank you. Tag has got a unique perspective on, uh, life and, Um, mental health and I cannot wait for you to share it with, with our audience. Tag, why don't you just share a little bit about, just summarize your life for just a bit and then we'll get knee deep into kind of what has changed your life significantly.
That sounds like a great idea. Um, I'll, I'll keep this brief So As a young teenager, I was diagnosed with pretty severe depression, and I'd been fighting it for many, many years.
I had learned to live a relatively normal life, went through school, held down jobs. And tried many different things, including medications, um, that helped to certain degrees or, or other. About 10 years ago, I was, uh, diagnosed with cancer for the first time and, uh, went through a fairly, uh, detailed and traumatic experience with, with that, as a lot of cancer patients do in their journey there.
And part of that is when I came out of it, I was, um, just hit a new low. And I was dealing with some psychiatrists who specialized with dealing with cancer patients. The doctor recommended that I look into TMS as A potential treatment for not just the long term depression, but also what I've been going through with the cancer treatment and how that had exasperated the whole problem with me.
I was up for it. I'm always willing to try something new, potentially, if it could be helpful for me, especially after coming off of cancer treatment, Didn't seem so bad. Real quickly, can we go back because you had said that you had struggled with depression for really the majority of your life and that you've tried, tried several different modalities of trying for treatment.
How successful were those for you? Were they because, you know, to try something new? leads me to believe that maybe they weren't the best. So I'm old enough that I remember when Prozac hit the market and I was on, well I went on Prozac and then variants thereof and those were really sort of the most helpful.
That would have been in the, I don't know, about 30 years ago and those helped in the sense that my depression did not get worse, if that makes sense. I had one. Psychiatrist, talk about how it was like sliding a board under your feet so you wouldn't sink farther. Oh, wow. Well, that doesn't sound great. Well, compared to where I could be going, it was a help, right?
Okay. With a lot of those drugs that came out in that era, there were a lot of side effects. Some of them were physical. Some of them were more sort of mental, cognitive. Type things. And I would struggle with those to the point as, a 20 something year old young man who didn't go to the doctor would sort of go, I'm doing better now.
I don't like being on the medication a whole lot because my brain is sort of foggy. I was having a hard time sleeping or I was sleeping too much. And so, you know, some of the, the effects of those medications were too similar to being depressed where. It takes energy to think and then straighten out your thoughts.
You sleep a lot or you don't, um, as, as may be the case. The only difference was I wasn't getting worse, if, if that helps. And for me, depression has been cyclical. I think my resting state at that time would have been for most people like pretty bad depression, but it made me functional and that was good enough.
Wow. Okay. So I know we weren't going to go here, but I am now, this is how it goes. Tell me what functional means when you have depression. What does it feel like? Well, to give an example, like, well, let me give you a couple of examples, right? So I'm going to start off in college, which is a special time at the typical college age where you're probably sleeping a lot and at weird hours.
Anyways, but I was doing that constantly getting to classes, uh, was a lot of effort for me more than just sort of, oh, I'm too tired or I'd rather go hang out with my friends. It was literally like, uh, a battle with myself internally to get out of bed, go shower, force myself to get something to eat, go to class.
And when I got pretty good at that, forcing myself to do that, but everything else that you would experience in that sort of age, like the social side and all that suffered, right? Because I was spending all my energy just doing the basics. And then when I had it left over, I would do my work and because of the depression and the mind fog and all that kind of fun stuff, it would take me a lot longer to get through my things.
I was also found that I needed to focus on one thing at a time. I couldn't multitask, uh, at all. So it was. Messy. Yeah. Um, it was highly focused when I could be and it was just an extraordinary amount of energy that I needed to expend to get through the day and, not fail my classes and graduate eventually.
But that was on the medication. You still felt like that. Good. So if you imagine sort of walking through like a swamp and it just gets, yeah, every step is an effort. What the medication did was.
You know, where I was slogging through this mess that was up to my, almost my hips. The medication prevented it from going up to my armpits, it's, uh, one way to think about it. I think it, it was easier than it could have been. If I hadn't been on the medication, I probably wouldn't have finished.
I wouldn't have been able to complete my classes or, or get through all that. So that's, that's the difference. I think there's a misunderstanding that it's a. The silver bullet and you're, you're sort of clear of depression. Um, you're not, it's just helping you function, get through the basic stuff that you need to get through.
And, for me it was, it was sort of the bare minimum that I needed to do to make my way through my education at that point.
The rise of Prozac started to get more attention into depression and that particular area of mental health where people became more aware of it.
I noticed a change, um, slowly over how people treated me at that point once they understood. You know, the majority of people still don't, if you haven't experienced or don't have a loved one that's experienced depression, it's really difficult to understand what it's actually like. 00. 05. I agree. I agree.
And that's why I hope that more people can talk and share their story so that you don't think it's just somebody who's sad. It's not that. There's so many more levels. I mean, I think it's worse, right? It's worse. It's, it's a lack of feeling. Yes, you feel sad, I guess, but it's not like, you know, sad, oh, my pet goldfish died.
Right. It is something that is just dragging you down. It's like this huge weight. It's just, there's no rhyme or reason. And you can't nail it. You blame yourself. you get the, I don't know, I know things have changed enough in the mental health field nowadays, but you know, back then it was just, Oh, he's lazy or he's not motivated or something along those lines.
It's, it's, it's, uh, stuff I grew up with. That was pretty much the diagnosis at the time. Well, and Tag, I think that while some of it has changed, I still think there is this, sadly, this perception, unless you are aware that the person is struggling with something, there is this initial perception that that person, it's, it's a character flaw.
Because, one, people still don't want to just share what's going on, right? And so they're looking at it as a character flaw instead of really an internal battle with an illness that is creating, these, these feelings and these challenges.
Yes, but okay the nice thing is the beautiful thing is so you you've you found a woman and Got married. So there must have been some relief and you have two children So you're raising a family now with still a depression that really isn't really solved, or you just still have that board under your feet?
Yeah, very much so. Um, as I said, it's cyclical for me. Okay. So, when I met my wife
and, and I actually had a few years where I, I was on a minor dose of medication and it was great, things were going well for me. I had taken on a job that, um, I had no background in and was self taught.
And a small but really strong group of friends, um, that understood me and my wife got me. even before we got married,and, things change. It came back. She saw me taking a dip and raised the red flags at that point, which was about the coolest thing I ever experienced, um, initially in our marriage, right?
Because there was somebody really watching out for me and it was like, whoa. Um. Oh my. Okay. That brings tears to my eyes. That is. One of the sweetest things I've ever heard, because to be seen and to be accepted. Right. I'm not saying like, you know, Hey, this marriage was easy and it was great, it was a difficult time and we've gone through difficult times since then.
you know, that was a moment of like, wow, this is amazing. And it's about the time. where I started seeing therapists on a much more regular and structured basis. I understood from my experiences previous to that, that I needed to find the right therapist.
So it took a few years for me to actually find somebody that I connected with and whose methods and approach clicked with me. Sure. It's a very personal relationship, isn't it? Incredibly. Yeah. And she's taught me a lot. I have a bag of tricks, a set of tools that is just huge now that I use constantly, even.
Now, where I'm not feeling depressed, um, all the time, um, that have just been like self care, sort of mental health tricks that keep me going. I've kept me going through some really rough stuff. I find myself doing some of these things, uh, like, uh, mental checks and stuff with how I'm actually doing what's going on in my head, almost unconsciously at this point.
And I've got to be. You know, people say, Oh, you should take medication or even the TMS in parallel with, um, actually a structured, uh, you know, time with, with a therapist of some sort or another. Um, I couldn't agree more. This is not, um, there is no single solution. There is no real solution for, um, most mental health issues, especially depression.
You know, when we first were trying to figure out what was going on with my son, you know, he's 11, I'm scared to death to put him on any kind of medication, but his, his situation was literally overnight and we didn't know what the heck was going on. But I had a psychiatrist tell me,
Andrea, you need the medication, or he needs the medication, to quiet the chatter in his mind so that he can do the work that therapy provides.
And at this point in his life, That chatter is so loud that he can't work efficiently with therapy. And that always kind of stuck in my head as, as so important because I think there are levels. of mental health issues, right? That where you can maybe just go to therapy if the chatter isn't too loud. But if the chatter gets really loud, you have to do both and you can't just take the medication.
Because then you're not changing the behaviors, so they, they've kind of got to go hand in hand and we'll talk about TMS in a minute, but like I always do, we kind of go off on a tangent and I'm, I'm now interested in kind of this whole depression thing. So anyways, um, so, okay, so you, uh, had a great therapist.
Sorry, I didn't mean to interrupt you there. Still do, still do. She's still amazing. I, I, you know, still have regular appointments with her. Yeah. And we talk about anything, it's, it's changed. I think there's a, I've got some interesting stories post TMS, um, that we can get into in a little bit, I think after.
Okay. Yeah. I would love that. So, okay. So you, you got this marriage and, and Gwen, who was a guest before is a very special woman and I was so impressed with the way that. that your family operated because your children also have some mental health struggles. Is that correct? That is true. Um, and, and in fact, they have both gone through TMS at this point.
Okay. Okay. And then as a father, who struggles with mental health. Did you start noticing things that were maybe red flags with the kids as they were growing up and and maturing? Oh boy. Um. I know. That was a side. I told you I went on a side track. I now am like thinking of the, from the father's standpoint and the, and your whole depression standpoint.
So sorry. Yeah. So with our, our firstborn We were getting feedback from preschool, kindergarten, you know, the early years of grade school from teachers of, uh, behavioral issues, not, like acting out physically or, or anything like that. And I've got to say, even with my personal experience, and if you go back far enough, I actually worked in the mental health field.
I did not see those things. I, I had my, uh, dad blinders on, right? Nothing's wrong with my kid. What are you talking about?Yeah. Well, and as a parent, you don't know anything anyways. Right? No, it's all new. Yeah. You're like, Oh, this must be normal kid behavior. I mean, how do you know? Well, right.
And we didn't see it, um, to the degree that the, the teachers were seeing it, uh, quite honestly. And, home was a safe space. So It was an easier place for them to be, uh, at that time, and they were more comfortable there. So there wasn't as much acting out. They, they seem like your average young kid, pretty much happy playing, you know, a little goofy, nothing terribly abnormal.
So it was very easy to ignore that feedback initially. We heard it enough that we sort of kind of had to look into it deeper and we did a bunch testing and many, psychiatric and, uh, psychology groups and so forth with that. And, indeed the teachers were correct. And, you know, that was for me, I was going to say initially, but realistically, even, even now, there's moments where I'm just heartbroken.
They, you know, have these things like depression, anxiety, which is not something that I have a large amount of. But, very, very serious forms of social anxiety and all that was, was, uh, you know, hard to take it. It hurt a lot. Well, cause you know, at least from the depression side, what it feels like, you know, the, those parents like myself who don't.
We can't relate to what the child's going through. So it's scary and we're sad for them, but we have no real basis of understanding the true suffering that they're going through. I would say that's even the same for somebody like me. Uh, you know, the, the, the perspective that I have is that I understand that how my brain works and why I'm depressed.
are at some level unique to me and perhaps I had the perspective of understanding that it was unique to each of my kids as well. What they were experiencing, what they were feeling, what was going on in their head was going to be different from what my experiences have been. Okay. And. I see that in their personalities, right?
These are not copies of me. They are two wonderful individuals with very strong, independent personalities. So they're, they're experiencing something different than I ever have while trying to get through this and as parents, what we try to do is support them as best we can, look for the opportunities, I think, um, we went through this with Gwen actually, and try the different approaches.
So. We're being as supportive as we can be with the information that we have, you know, again, different era growing up, I was lazy, uh, you know, I'm hoping that with my kids growing up, it was like, okay, they are fighting these mental health issues. And this is why, uh, they're, they're, this is where their energy is going.
This is what they need to focus on. As opposed to, oh, they're lazy, you know. Well, I mean, you're coming from a perspective of knowledge, first of all, right? You have much more knowledge and you have a lot more empathy. Right. The, the empathy piece I think is, is huge and their environment is so much more loving than probably you, you've come from.
Not that your family wasn't loving, but even the people surrounding them, they've got an advocate in their parents who know things. We are allowed to talk about it a little bit more than when you were a child. So you know, they're coming from a place of a little bit better understanding. Right. And this is where things have changed, um, and you know, societal changes where we're more accepting of these, uh, diagnoses.
We're more aware of the various diagnoses. It's you look at how they can be broken down for various mental health issues much more succinctly than 30 years ago, 40 years ago where it was a sort of you were tossed into one of a handful of buckets. Right. And now it's, it's. A lot more focused, there's a lot more understanding and it's a little scary because the farther the researchers, everybody digs, the deeper it goes, the more, you know, it's, but it is a better place where you, to support people.
So, this is kind of a good moment to switch, I think, to TMS because you're talking about researchers and being able to find different modalities of treatment. And that's how, after talking to Gwen and understanding your story, I really wanted to talk to you because You were, uh, introduced to something called transcranial magnetic stimulation, TMS, which is a newer procedure in the whole sense.
I mean, it's been around for a while, um, but it's just kind of, at least here in California, it's just kind of hitting mainstream. I know that I am a huge proponent of this because my daughter was able to partake in it last year when she turned 18, and it was a game changer for her. Prior to that, she had been on probably 15, 16 different types of medications or cocktails of medications, she had done biofeedback, she had done just a whole slew of different things and nothing ever worked for her.
And she did TMS and luckily she was one of the 60 or 70 percent of the people that it worked for and it changed her life. It literally changed her life. So I want to share what TMS is. Is, and how it works and then get into like the details and like feels and that kind of such.
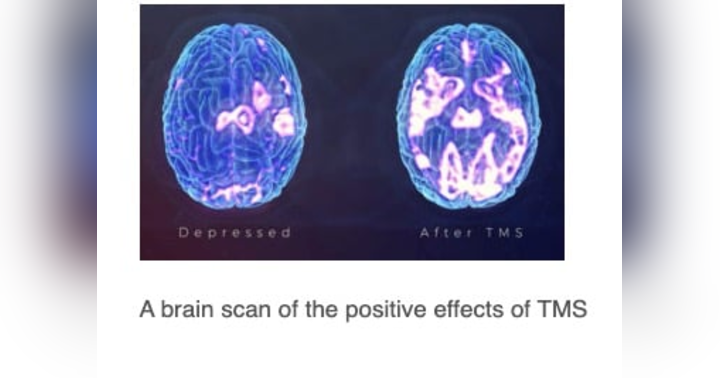
I know. Nice of you. Yeah. Yeah. Yeah. Okay, so it's kind of funky in some ways. TMS is not electroshock therapy, as we were discussing earlier. It's not scary by any means. It is a highly focused magnetic pulse that's sent to a very specific area of your brain that helps the brain remap some of the synapses to overcome depression.
So Depression happens to be one of the first major. areas that they're targeting with, with TMS. They're starting to target more and more with, um, like severe anxiety issues is my understanding. And there's some cutting edge newer pieces they're looking at that cover a whole wealth of different areas that are really interesting.
I had actually heard too that it was started with depression, PTSD, it's supposed to be very effective with, and actually OCD. So those three I think the FDA has approved it as a treatment and now they're expanding it to various other parts of the brain. Yeah, the more research goes on, it's, it's expanding as to what can be done, um, as, as they understand how the brain is mapped and all that.
It's, it's really fascinating stuff as far as what they're discovering along the way. Yeah. Now you mentioned that it's not like electroshock therapy. It's actually non invasive at all, right? There's like, you don't feel it at all, right? Well, sort of. Okay. You know, electroshock therapy in, in sort of the modern psychiatric sense is, is not the same as what we think of from the, the movies from the 1950s and so forth.
It's very different there, um, but that's a different story. Uh, this. Speaking of the 1950s, they sort of fit you with a helmet that looks like it's out of some 1950s space age, uh, thing. Um, it's just a big clunky plastic thing with a tube coming out the top or the back and they, uh, sort of shuffle it all around, make, uh, markings on this little skull cap that you wear.
So that it sits just right and targets a specific area. It then, when they kick it off, sends out little pulses. And it's, it sounds a little bit like if anybody's had an MRI, that sort of like thumping sound. Um, but like think of it in a, not as loud. Okay. You know. What it feels like is if somebody is sort of, you know, taking their finger and just poking you in the head every time there's a pulse.
Um, at least this is what it felt like for me. It was, it was sort of like somebody snuck up behind me and was going, tap, tap, tap, tap. Are you there? You know, like, um, and that was about it, like physically that I felt while it was happening. In all honesty, I sat there with the technician most days and we watched YouTube videos.
For half an hour, that was it. Then I'd drive home. There was no pre medication, no post medication. For me, initially, I'd say for the first three of the six weeks, I'd come home and I'd suddenly be really tired for a little bit, but then I'd come out of it. Probably because your brain was like working out, right?
Like it's, I mean, if it's remapping, it's almost like it's working out the brain. I guess. I don't know. You know, my younger child experienced the same thing. She also, they also went through it and would get tired afterwards. My older child, nothing. No problems at all. And then, you know, so you wear this goofy helmet in a small little room with this thing tapping and making noise and that's all there is.
It seems like science fiction. And I, when it was recommended to me, I told the psychiatrist, I'm like, I'll try it because I'm open to trying anything. But this doesn't sound like something that would actually work. This sounds like science fiction, fantasy type of thing. And he's like, I thought that too, until one of my fellowships was at a TMS center.
And I saw it. Well, my daughter was like, she was angry at me the night before our first treatment. She was mad at me. She did not want to go. She, I mean, rightfully so, right? She had been through 16, 17 different medications and who knows how many other things and nothing worked. She didn't want to get her hopes up, but she was, she yelled and said, I'm only doing this for you.
And she did it. And I will tell you that she actually was that doggone stubborn almost through the entire 35 days of treatment. And then at the end, she changed. My eldest fought through the same sort of thing also. The difference is, I've had a lifetime of this. I had just gotten off all that cancer stuff, um, so, you know, at that point, what's the worst that could happen?
Right. Right. I've already been through some pretty bad stuff. Which, by the way, I don't want to make light of the cancer stuff, that, I can't believe all that you've been through, Right. I mean, are you interested in a brief timeline on that, or? Yeah, let's do it,
Okay, so, um, diagnosed with, with cancer. Of course, a surprise, nobody expects cancer. I went through excellent program here in Boston. They got me into remission after a bunch of chemotherapy, which was not easy to deal with. I experienced, you know, a fair amount of side effects, some worse than others. At that point, I did not lose my hair.
Uh, if anybody's who's interested. Shortly after I was in remission, my wife was diagnosed with cancer as well. She went through the surgery, uh, radiation, and chemotherapy process. Went into remission, we had about a year, and my cancer came back. And at the same time, they found the second much rarer form of what I had.
So I had two types of cancer this time. That time was chemotherapy, much more aggressive than the first time around. I had to be hospitalized because the process was 12 hours to receive the chemo and the infusion center was not open for 12 hours at a shot. So I'd go in every couple of weeks and get that.
I then went to radiation to do that. Then I was put on the list for a stem cell transplant, which is effectively most bone marrow transplants are now stem cell transplants, um, for, for cancer patients, which was a month in the hospital. They basically kill your immune system. Um, it's, it's awful. It's brutal.
And you come out just an absolute mess. You, you, I couldn't walk 50 feet without being exhausted. Uh, everything had to be. pristine clean because I had a brand new, uh, immune system at that time effectively. And it was six months before I could be around people other than my immediate family. Did you have to go off any other medication?
Were you able to treat your depression during this time too? I was. Thank goodness. Right? Yes. Um, I had very, uh, I had, uh, my, my oncology transplant team and my regular oncologist are superstars. They're spectacular. And they're the ones who set me up with a psychiatrist. Uh, they have a whole department at this particular hospital, which the psychiatry group treats cancer patients.
So, it's, it's specific. Is that common? That they would have that type of a, or do you know? I don't know. Um, we live in the Boston area, which is some of the best hospitals in the world. Sure. Yeah. Um, and, and practices. So, that, that is something where we're really lucky. And when I actually asked about, you know, well, why do you have, uh, you know, an oncology, a psychiatric oncology department?
One of the psychiatrists was like, well, because most psychiatrists would just go, ah, I don't know what to do. This is like too much. Um, so they, they, they monitored my medications and how I was doing. Um, and it's ultimately what led to the TMS was, was through that department. And helping me, uh, get through this and, you know, part of the cancer treatment isn't just all the awful things that happen to your body, but it's, it's, um, it messes with your mind.
I mean, quite honestly, it's, you know, your, your own mortality and your family and. All the other bits and pieces of your life are just turned upside down. It's an awful journey for not just the patient, but everybody around them who tried to support or be there in some way or another. So, They had gleamed obviously on to that, uh, the mental health piece was, was important and they were very excited that I had a, you know, a longstanding therapist already and was continuing to see them to work through some of that.
You know, that's sort of the genesis of what, where, where TMS came on the map. I was trying to get back to a normal life, uh, after. I was allowed back in public, um, the irony being that when I was finally allowed into outside public spaces without a mask is when COVID hit. Are you sure you're not donned in like a red jumpsuit and a cape and coming out as Mr.
Incredible with all of this? You
are. Amazing. Holy cow. Yeah. So everybody complaining about masks, I'd been, it was so easy. I'd been doing it.
It was a shock. Uh, I tried going back to work part time to, to give me something to do. Realized my cognitive ability had just. Nosedived. I couldn't think through anything. I, you know, was expected to solve complex problems and I could barely solve basic problems. Um, a lot of things had happened because when you, you know, on the stem cell transplant with all the chemo and stuff leading up to it, I couldn't work.
Literally. That, that Sort of made everything spiral even more. Um, so I was dealing with, you know, all the questions of my mortality. What have I been doing in life? All these sort of, uh, existential, uh, things going on, trying to get back into work, getting dinged at work because I couldn't, you know, produce like I used to, and I just crashed in all honesty.
I was just. That was it. And I was in touch with my psychiatrist and he's like, TMS, you need to look into this. So we made some adjustments to the medications I was on. Nothing big. And I looked into TMS. Much like your daughter, it was life changing for me. How quickly did you start seeing results? So apparently I'm quite unusual.
I am one of the very lucky few. Well that's, that's beyond even just the TMS piece. I am in a positive way for once. I am pretty sure. So I started responding within about two weeks. Uh, less than 10 days. I mean, it was fast. Wow. So you felt it within 10 days. You felt a difference. Right. So, I wasn't sleeping, for example, um, because of the stress of, of where I was mentally with my job, with my health, all the other things.
I, I couldn't sleep. It was just too much going on in my head. I started sleeping through the night and, and waking up rested within the first 10 days was the first thing. Um, so that was just mind boggling to me. I was skeptical and hopeful at the same time at that point. And then it got better. Like I could handle multiple things going on at the same time.
You know, I hadn't been able to do that since I was first diagnosed with cancer. And things started to sort of focus in my head a lot faster and a bit more clear, so I didn't have as much chaos going on in there. I was able to work through both internal, external, more difficult problems without sort of.
Just collapsing inward, and, you know, I could multitask for the first time in like 40 years, like properly. Wow. So for me, I am one of those very rare instances where it was just huge. Huge changes and quickly. Wow. It's been a few years and I'm still going strong with it. Like I haven't needed to go back and get a tune up as they say.
Yeah, exactly. Which is not uncommon. And it's, um, in all honesty, even if I did, it's not a big deal because as I said, you know, you. You drive in, you sit down on this chair, wear a funky helmet for 30 minutes, and you go home. Yeah, so my daughter, she did it last year. Mm hmm. And then, um, not as quickly as you, but it was a game changer for her.
And then she did need a tune up this year. And so she called and she drove down there and for her it was only five minutes. She literally drove 40 minutes, sat in the chair for five minutes and then drove back home and she's back to, you know, it's just, it's, it's amazing, amazing, but unfortunately it doesn't work for everybody.
No, it does not. It is, it is, um, one of those things, but you don't, we don't know, the researchers don't know, the clinicians don't know enough as to identify exactly why that happens. And why it works for some people more than others, you know, I don't know if it's that I'm older and I've experienced things and I'm, uh, better attuned to where my mind and body is than maybe a teenager.
But, uh, it could just be how my brain's wired, or was wired. But it worked for your children. So it was such a good thing for you, you decided to introduce your kids to it. Well, yes. With our eldest. That's, that's, that's what we did. And, um, as I said earlier, we're very resistant to the whole thing and kind of holding it against us all the way to the end.
Still doesn't admit that it did any good. Oh, really? Oh, yeah. Those teenagers are so stubborn. Uh, but we noticed the changes. And we still notice the changes. It's been over a year for that child, the younger one. requested it because they had seen my changes and they had also noticed the changes in their older sibling.
And they said, well, you know, if I'm depressed and I've got a bit of anxiety, can I try it? You know, okay. Yeah. The state just allowed younger, you know, sort of mid teenagers, they're 16 to do it. So there we go. And it worked. The response for them was not as rapid as mine. Um, but the depression wasn't as deep either, so.
goes that part. But there was anxiety wrapped up as often as the case with depression and anxiety go hand in hand. The school year has started off and it has been the best start to a school year we've had with, with this child. They are working hard, doing well, having a good time, looking, you know, forward to college and actually researching what they want to do.
do in college and which colleges offer it and, um, I'm just, uh, you know, sort of blown away by that. Yeah. Yes. It, it helped both of them, whether they accept it or not, um, which certainly do. And, uh, you know, for me, uh, it's just, as I said, life changing.
I mentioned earlier the story of my therapist at about three or four weeks into TMS. I sat down with my therapist and we discussed what we wanted to talk about that day, what was sort of on my mind and, okay, so you've been wonderful at helping me get out of crises, you know, with my, my mental health and, and working this, you know, coming out into a sort of normal or, or having the tools to work through a more normal life.
And it's been wonderful and absolutely amazing. My problem now is that I have the bandwidth, the interest and, you know, the, the general energy that I can do a whole bunch of things at once. Like it's no longer like, what am I capable of like realistically for the next day, week, whatever. I suddenly have all these things and I don't know what to do with myself.
There's too many choices. How do I handle this? It's, it's sort of like going to see the therapist for the flip side for me. Right. Oh, that's fantastic. Yeah. Uh, it was, it was new for both of us,
but it was interesting and, you know, we, we, we, we still talk about that. You know, these few years later, and they're quick to remind me that where I've come from, what I've been through, if I'm having a bouncier, you know, sort of a rougher day or a week or whatever, all honesty, I'm at the point where I already recognize that, you know, I can reflect on this stuff and go, Oh, this is where I was.
This is what was happening and, and a whole lot of details around it. This is not something I could have done easily before the TMS. You know, honestly, the medications weren't doing this for me, right? So this is life changing that I'm able to reflect on some of the ugliness and take away the positives from it.
You know, I don't, I don't sort of, uh, have a perseverance around the negatives all the time, which is just sort of feeds the depression. I'm able to break those loops now without putting a ton of effort into it. What a wonderful perspective. I mean, think of you said in the last 20 minutes that at one point in your life, you were questioning your own mortality, right?
And you were in like the lowest of lows. And then now you're looking at everything with such hope and joy. I mean, what a beautiful, you know, transition that you've been given. Well, there's, there's a lot there. There's a lot of stuff that you could unpack about me mixed in with that. Right. So the, the, the TMS was one piece in all honesty, the seven, eight years of constant cancer stuff in the family certainly changes your perspective.
When I was getting the stem cell transplant, you spend about a month in the hospital. You're pretty heavily isolated because of. You know, no immune system and you're also insanely sick because they're basically trying to bring you as close to death as possible before they give you. The, the, the new stem cells.
So there's time to think in those moments of consciousness while in the hospital. And there was a lot of introspection I did, a lot of sort of thinking about what I had done. Again, this is that sort of existential crisis type of thing, but also a lot of what do I want to do and where do I want to be?
What's important to me? I made decisions at that time that I've since followed through on some of them, but they happened post TMS that really sort of shook things up and put me in a better place. Mentally, in a lot of ways, even without the TMS. So, one of the things is I'd always wanted to go back to school and get my advanced degree.
I wanted to go back to my roots that were more in psychology and arts and all that. When I hit that low and when I had the TMS, I came out of the TMS and thought, Yeah, I, I need to do this. I need to make this big switch. So since then, I have gone back to grad school and graduated, um, in a totally different field.
Loved every minute of it. Heck, I, I academically did significantly better than I did as an undergrad at 20 something. Um, I'm, I'm headed down a path that I am much more comfortable, much happier about. And it was a buildup of all those things with the TMS giving me that final push to actually be able to do this, studying for eight hours every day plus hours, doing the work I needed to do.
I'm not sure I would have attacked it with the same vigor and interest. Even if it had been the same thing, something I'm really interested in and love doing. You might not have had the ability to do it. I mean, it would have been so exhausting based on what you had said before. Exactly. Yeah. So, it's a very different place.
And, I recognize that my depression is not gone, per se. I recognize that I'm still dealing with side effects from all the cancer treatments. and some of those have been cognitive. And, that has become clear because I have the ability to sort of mentally manage this and because I'm able to do that.
It continues to put me on a good path forward. So, I would have focused on the negative things that happened. So, like, I've been dealing with, um, long standing, slowly improving cognitive issues. Like, I haven't been able to think as quickly or as clearly, since the chemo, especially, just made everything, you know, 10 times worse.
So, that's still clearing out for me, I, I had a moment of realization a couple of months ago about that and I was just like, Oh, yeah, the difference is that I went, yeah, give myself some room for that, as opposed to. I'm never gonna get out of this and just sitting in that endless circle of like how awful I am, how lazy I am, all that kind of fun stuff that others and you tell yourself or what you think others have told you, um, that depression, distorts that reality and I've been able to get out of that.
And that's really what the TMS did for me, is it allowed me to break those cycles and develop new behaviors that have been absolutely life changing. It's why we supported my kids going through it, because the risk is just so insanely low. Um, and the odds of it working are, are decent.
It's worth the shot. But it's worth a shot. I agree. It is super low effort. you spend more time in the car quite often than you do at the appointment. That was true with us, yes. That was true for, for all three of us here. Tag, you don't know how grateful I am for you sharing this. I mean, I, I do have a little bit of a tear coming out.
But I just. I, I am so grateful for you and your family and all that you've shared with us. And I hope that one, you continue to see joy, hope and happiness in your life. And then also I hope that we are able together to get this message out to, to anyone who, who can benefit from it.
Thank you. Yeah, it is. It is. It's a wonderful thing. Um, if it, if it works for you, it's, it's life changing and it's worth the risk because unlike the medications, there's not a whole lot to go wrong. No, there's not. There's not.
Thanks for tuning into this way up. I hope you're feeling a little lighter. A little brighter and ready to take on whatever comes next. Remember, the journey of mental health is all about progress, not perfection. So keep climbing, and don't forget to celebrate the small wins. If you enjoyed today's episode, be sure to subscribe, leave a review, and share it with someone who could use a little lift.